A 22 year old female from thipathi came with c/c unable to pass the urine
N.lavanya
Roll 93
This is online E log book to discuss our
patient’s de-identified health data shared
after taking his/her/guardian’s signed
informed consent.
Here we discuss our individual patient’s
problems through series of inputs from
available global online community of experts
with an aim to solve those patients clinical
problems with collective current best
evidence based inputs.
A 22 yr old female from Tipathi , farmer by
occupation
came to the opd with
Chief complaints
Fever since 10 days
Head ache since 7 days
Unable to pass the urine since 2 days .
History of presenting illness:
Patient was apparently assymptomatic 10 days
And developed Gradual onset High fever with
chills and rigor continuous associated with
nausea , relieved on medication
she had c/o Headache , diffuse in
region , occipital region predominantly, Gradual
in onset , dragging type , radiating to neck ,
Aggrevated on talking , rotating the head ,
relieved on medication
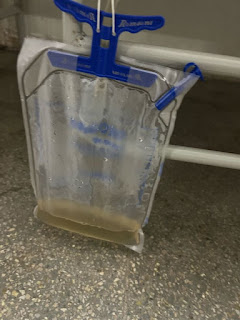
c/o urinary retention ( acute ) for 2 days
Able to feel the fullness of bladder , not able to
pass urine , relieved after passing foleys
Had Weakness of lower limbs for 4 days .
Spontaneously resolved .
- patient was not able to walk on her own during
the weakness episode
- No seizures
Past History:
The patient had a similar episode one year back
She had high grade fever for one month gradual
onset continuous type associated with head ache
nausea weakness of the limbs and blurring of vision
Symptoms relieved on medication
5 days after the onset of the fever patient was
unable to pass the urine for 2 days and had an
episode of
Altered Sensorium which lasted for 5 mins . Not
able to recognise persons , place, time .
Past history:-
Not a k/c/o DM, Asthma , Epilepsy , HTN
Menstrual History :
Personal history:-
Married female
Appetite - decreased , improved since yesterday
Bowels- Constipation , relieved on medication
Micturition- abnormal
Addictions:- No addictions
Family history:- Not
General examination
Vitals :
Systemic examination :
Abdominal examination
Inspection
Neck stiffness:- No
Kernig sign :- No
Sensory examination:
Right Left
Spinothalamic
Crude touch + +
Pain + +
Temperature + +
Dorsal column
Fine touch Lost in bilateral soles
Vibration
Olecranon p 6s 5s
Styloid process 7s 10s
Tibia 4s 8s
Medial mallelous 6s 10s
Motor examination:
Tone. :- Right. Left
Upper limb. Normal. Normal
Lower limb. Normal. Normal
Power. Right Left
Upper limb. 5/5. 5/5
Lower limb. 5/5. 5/5
Reflexes. :- Right Left
Biceps. + +
Triceps + +
Supinator. - -
Knee. ++ ++
Ankle. ++ ++
Plantar. Flexor Flexor
Lower limb examination in detail, done to localise anatomy of lesion:
Power. Right Left
HIPS
ILEOPSOAS (L1-L3) 5/5 5/5
ADDUCTOR FEMORIS (L5-S1) 4-/5 4-/5
G MAXIMUS (L5-S1) 4-/5 4-/5
G MEDIUS, MINIMUS (L2-L3) 4-/5 4-/5
THIGH
HAMSTRINGS (L4-S1) 4-/5 4-/5
QUADRICEPS (L3-L4) 4+/5 4+/5
ANKLE
TIBIALIS ANTERIOR (L4-L5) 4-/5 4-/5
TIBIALIS POSTERIOR (L4) 4-/5 4-/5
PERONEI (L5, S1) 4-/5 4-/5
GASTROCNEMIUS (S1) 4-/5 4-/5
FOOT, GREAT TOE
EXT. DIG. LONGUS (L5) 4-/5 4-/5
FL. DIG. LONGUS (S1, S2) 4+/5 4+/5
EXT. HAL. LONGUS (L5, S1) 4-/5 4-/5
EXT. DIG. BREVIS (S1) 4-/5 4-/5
- No finger nose in coordination
- No knee - heel in coordination
Investigations:
Hemogram:
Hb: 9.3 gm%
TLC: 6700
PCV: 29.8
MCV: 71.0
MCH: 22.1
MCHC: 31.2
RBCs: 4.20 millions/cumm
PLT: 3.63 laks/cumm
USG ABDOMEN AND PELVIS
Provisional Diagnosis:
LMN Type Neurogenic Bladder
?Recurrent Transverse Myelitis
?Neuromyelitis Optica Spectrum Disorder
Treatment
Ophthalmology opinion was taken for this patients.
Impression: Normal fundus study.
Advice:
1.E/d LUBREX 5 times/day
2.Use glasses(Myopic glasses)
Neurology opinion was taken on 29/6/2023
and she adviced-
1.Inj.METHYLPREDNISOLONE 1gm in 100ml of NS once a day for 5 days.
2.Inj.Pantocid 40mg OD/BBF for 5 days at 8 AM
3.Tab.AZORAN 25 mg once daily at 2 PM
4.E/d LUBREX 5 times/day FOR 5 days
progression
We started giving 1gm METHYLPREDNISOLONE in 100 ml of NS under observation, And on the 3rd day she passed urine(Foley's catheter was removed)









Comments
Post a Comment