A30 yr old male AMC 3 bed
Roll 93
This is online E log book to discuss our
patient’s de-identified health data shared
after taking his/her/guardian’s signed
informed consent.
Here we discuss our individual patient’s
problems through series of inputs from
available global online community of experts
with an aim to solve those patients clinical
problems with collective current best
evidence based inputs.
Chief complaints:
Involuntary movements of hands and tingling and numbness in upper limbs and abdomen since 1 day
History of presenting illness :
Patient was apparently asymptomatic 20 days back then
He developed fever insidious in onset, gradually progressive, low grade , intermittent not associated with chills and rigors and relieved by medication
He has a history of 4-5 episodes of vomitings 5 days back. Watery, non bilious ,non projectile, with food particles as contents.
And had a history of visit to nagarkurnool and consumed food there and due to water change patient also had hoarseness of voice
Relieved by medication (unknown)
No c/o pain abdomen, loose stools
c/o burning micturition 2 days back, relieved now
H/o similar complaints in the past(7 years back) (hypokalemiac periodic paresis)
No h/o DM,HTN, asthma, epilepsy,cad, thyroid disorders
He used to take alcohol occasionally for the past 10 years and stopped taking 1 month back
He takes tobacco once in 2 days for the past 10 years
Patient is not co operative to let me take clinic images of chest and abdomen
O/E
Patient is conscious, coherent and cooperative well oriented to time ,place and person
No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy,edema
Vitals:
BP - 100/70mm hg
PR- 86 bpm
RR- 16 cpm
CVS EXAMINATION:
S1,S2 heard no murmurs
RS EXAMINATION:
trachea central
NVBS +
BAE +
P/A EXAMINATION:
Soft, non-tender
Bowel sounds heard
CNS EXAMINATION:
Hyporeflexia (due to hypokalemia)
Serum electrolytes
Na - 139 mEq/L
K -2.3 mEq/L
Cl - 95 mEq/L
Ca - 1.01 mmol/L
Mg - 2.0
Urinary electrolytes
Na- 162
K - 7.3
Cl - 123
Urine Ph - 7.0
Serum electrolytes :
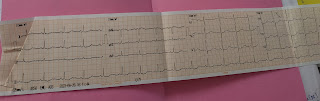
ECG
Xray chest PA View
Consolidations in the left upper lobe
B/L hilar shows normal in size
Trachea central in position
Cardiac size is normal
Right lung shows normal translucency
TREATMENT:
1)Inj. Kcl 50 mEq in 500 ml NS / IV over 5 hours
2) Inj. Zofer 4mg iv/OD
3)Inj. Pan 40 mg IV/OD
AMC-30 YR M
C/O PAIN ABDOMEN
ON EXAMINATION:
PATIENT IS C/C/C
TEMP: 98 F
BP:100/70 mmHg
PR:86 BPM
RR: 16CPM
CVS:S1,S2 HEARD ,NO MURMURS
RS:BAE+,NVBS, NO ADDED SOUNDS
P/A: SOFT, NON TENDER
CNS:
TONE NORMAL IN ALL LIMBS
POWER 5/5 IN ALL LIMBS
A:
HYPOKALEMIA UNDER EVALUATION And pulmonary tuberculosis
And kept on anti tubercular drugs










Comments
Post a Comment